Recommended

Blog Post
No healthcare system has an unlimited budget, and policy makers everywhere must balance demand for new health services with finite resources. Priority setting systems, often in the form of health technology assessment (HTA), can help evaluate whether health services provide good value for the money spent. ‘Full’ HTA assessments demand substantial resources to produce locally relevant evidence for decision making. However, there is a disconnect between the time that full HTA takes, and the pressure that policy makers are often under to make decisions quickly. In some instances, it is useful to borrow from the many assessments and HTAs already completed using an ‘adaptive’ HTA (aHTA) method to improve the overall efficiency of HTA systems.
We are excited to share a comprehensive systematic review of existing global aHTA methods that we recently published in Value in Health.
For those unacquainted, aHTA is a method for weighing the costs and benefits of health interventions by adjusting full HTA for time, data, and capacity constraints. Often, it leverages HTA evidence from other countries, rather than full HTA which does all of the analysis from scratch. Our exploration of aHTA methods was motivated by our work in nascent HTA systems through the international Decision Support Initiative (iDSI), a global network of health, policy, and economics practitioners working to support the development of priority setting systems. While aHTA is practiced globally, there has been no clear overview of existing aHTA methods to date. Our review sought to fill this gap to improve aHTA methods’ replicability. In this blog, we summarize a few key takeaways:
aHTA is an established, worldwide practice
Guided by our previous definition of aHTA, we sought to find formalized aHTA methods in HTA agencies’ and networks’ protocols and guidelines. We found e countries/networks using aHTA, and twenty-one of them provided sufficient detail to categorize the methods. Most of the detailed methods were found in high-income countries, while those with less detail were from low- and middle-income countries (LMICs). Nonetheless, this suggests that aHTA is not just for LMICs, but is practiced alongside full HTA, to improve the efficiency and speed of HTA systems. Indeed, we found protocols that completed aHTAs in as little as five days, and a study of Ireland’s HTAs found that half were full HTAs and the other half were aHTAs, which saved 15,000 appraisal days.
Developing a nomenclature for aHTA is an important first step to ensuring its replicability
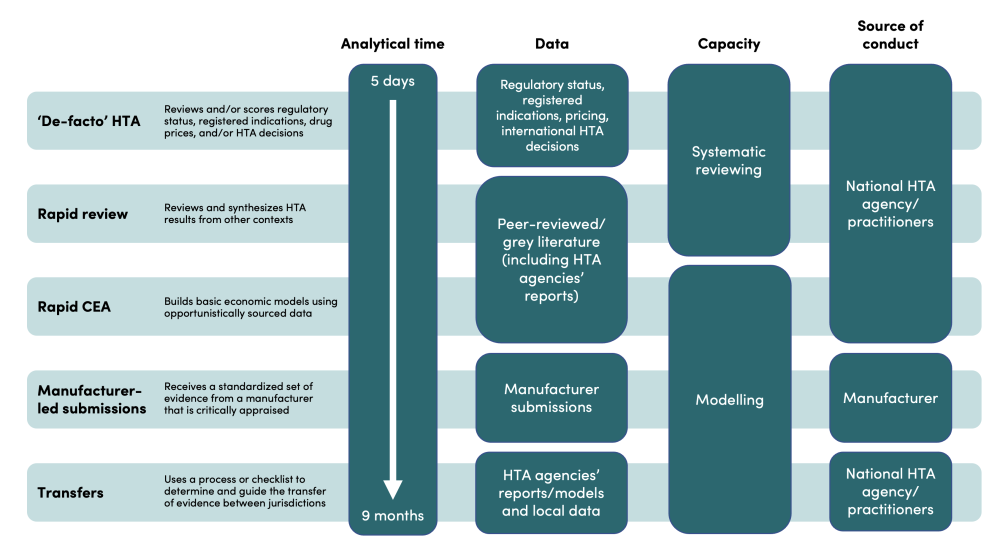
Our review did not find an agreed nomenclature for aHTA. As such, we have categorized aHTA methods into five ‘buckets’: de-facto HTA, rapid review, rapid CEA, manufacturer-led submissions, and transfers. An overview of each is captured in the illustrative figure below alongside brief definitions.
Source: Nemzoff et al.
An important motivation of this categorization was our own experience supporting Rwanda, Ghana, India, and Indonesia to do aHTAs. Each country was at a different stage of their HTA journey but had similar considerations to address. Policy makers were under pressure to complete HTA analysis quickly; local data availability was sparse to inform HTA analysis; and capacity to complete an HTA analysis was limited to small groups of health economist and clinicians. Through these experiences, there was a need articulate options for methods more clearly based on these considerations, so that stakeholders could choose the optimal method for their local context.
Urgency, certainty, and low budget impact can trigger the use of aHTA
aHTA is not appropriate for all health interventions. In our review, we found urgency, certainty of the evidence base, and low- budget impact were three recurring “triggers” that would make aHTA use more likely. Urgency allows policy makers to be responsive, while certainty and low budget impact allow policy makers to minimize the risk of a poor decision.
These triggers will vary across countries and could be entirely different in different contexts. Nonetheless, the triggers can be used to help guide the selection of methods and can even be used to “route” topics to aHTA or full HTA. For example, in South Africa; a rapid review is completed first and further analysis is only done if there is uncertainty linked to clinical effectiveness, cost, cost-effectiveness, or other factors.
More work to be done in the future
Our review found that, when appropriately triggered, aHTA is an important component of many priority setting systems. We hope that this review and its categorization helps to shift the paradigm on aHTA from relying on HTA experts to decide where ‘cutting corners’ is appropriate, to locally owning and guiding explicit methodological decisions based on a structured set of considerations. This is only the beginning, and more work needs to be done to establish, test, and refine the methods based on broad experiences from across the globe.
The full systematic review is available open access through this link. This review would not have been possible without the inputs of all co-authors including Hiral Shah, Lieke Heupink, Lydia Regan, Srobana Ghosh, Morgan Pincombe, Javier Guzman, Sedona Sweeney, Francis Ruiz, and Anna Vassall. Any queries about the review or its content can be directed to Cassandra Nemzoff at [email protected]
This blog and review were developed with various members of the iDSI network, including LSHTM (GHECO), where the blog has been cross-posted.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.
Image credit for social media/web: VectorMine / Adobe Stock