Recommended
Key Recommendations
-
Implement quick wins to re-establish US credibility and engagement in global health
-
Reverse life-threatening reductions in childhood vaccination and deliver COVID-19 vaccines to all with a G7 and G20 deliverable to launch a new era of preparedness and Protect Our World
-
Build an adequately funded global health security architecture that mitigates the impact of future disease and biosecurity threats on human well-being
-
Advance a health systems approach to funding and coordination of the trademark US global health programs in HIV/AIDS, malaria, maternal and child health, and family planning
- Address the fiscal and economic fallout from the COVID-19 pandemic
COVID-19 has elevated global health to the top of domestic and international agendas. But at home and abroad, the US response has failed to protect lives. Domestically, testing failures, mixed and incorrect public health messaging, inconsistent state-level policies, and erosion of trust in national public health authorities continues to fuel one of the worst epidemics in the world, killing nearly 275,000 Americans. Internationally, the US approach has been under-resourced and incoherent. Meanwhile, the pandemic has led to worldwide reductions in the coverage of essential public health interventions like childhood vaccination and HIV/AIDS treatment,[1] contributing to high numbers of excess deaths, and has magnified the inefficiencies that have long plagued the US global health architecture.
Global health goals must also reckon with the fiscal implications of the COVID-19 pandemic—at home and abroad. Americans have suffered deeply from the health and economic crises. Amid pressing domestic needs, the Biden administration and global health community must be prepared to show that US investments demonstrate results; that US engagement on the international stage remains critical to protecting health at home; and that gains abroad rebound to increase Americans’ own safety and welfare. And in many lower-income countries, COVID-19 is primarily an economic and fiscal crisis, and only secondarily a health crisis—so how the US government and the broader global health community handle this reality programmatically will be important for impact.
Against this backdrop, the US government remains the world’s largest global health donor,[2] and global health accounts for roughly a quarter of the base US international affairs budget.[3] Looking ahead, US efforts must demonstrate commitment to impact with equity, recommit to global cooperation, and encompass more than aid, harnessing opportunities to leverage the entire toolkit of US policy, influence, and institutions.
US credibility as a global partner is at stake
For most of the last four years, the Trump administration treated global health assistance as an afterthought, seeking spending cuts while pursuing a more transactional approach to foreign aid. This culminated in the Trump administration’s decision to abruptly withdraw from the World Health Organization (WHO), resulting in a loss of international credibility alongside a missed opportunity to develop a more coherent response to COVID-19 at home and abroad.[4]
The Trump administration also scaled down existing US government infrastructure designed to detect and mitigate infectious disease outbreaks, including by dissolving in 2018 the dedicated Global Health Security and Biodefense unit within the National Security Council and reassigning its directive to officials tasked with a broader nonproliferation and counterterrorism mandate.[5] Domestic antiabortion politics have hamstrung international efforts to expand access to sexual and reproductive health, through the proliferation of spending restrictions combined with attempts by senior administration officials to police the use of related language in multilateral communiques.[6]
The United States’ own inadequate and highly politicized response to the ongoing pandemic, both at home and abroad, has undermined its global credibility. Further, while the US has made significant progress toward development of a COVID-19 vaccine through the Trump administration’s Operation Warp Speed, it has largely recused itself from global efforts to ensure equitable distribution or diversify the portfolio of vaccine candidates.[7]
COVID-19 is erasing decades of global health progress
The current global crisis is not only about COVID-19 but also its collateral effects, particularly in the poorest countries, where it has disrupted essential services ranging from routine vaccination and HIV/AIDS treatment to dialysis and cancer screenings.[8]
Vaccination, the emblematic public health intervention where the US government has historically been one of the top international donors, is among the most vexing examples. Immunization has brought polio to the brink of eradication and led to a dramatic decline in measles worldwide; UNICEF estimates that measles vaccination prevented 23.2 million deaths in 2000-2018, making it one of the best buys in global health.[9] Still, US-supported vaccination programs faced challenges prior to COVID-19 that have been exacerbated by the current pandemic. For instance, vaccination rates generally were lower than necessary for herd immunity,[10] inequitable distribution remained a persistent issue,[11] and vaccine hesitancy and low uptake[12] had begun to erode demand. In 2019, there were over 850,000 measles cases reported globally, the highest number since 1996.[13] The US government has made significant contributions to combating the scourge of polio for nearly half a century,[14] but low levels of polio immunity and poor vaccination coverage have led to continued outbreaks of vaccine-derived polio virus, posing a threat to eradication.[15] All of these issues have contributed to an increase in preventable child deaths. They also suggest a range of obstacles that could undermine the ability of countries and communities to access an eventual COVID-19 vaccine, particularly where initially limited supply will demand prioritization of vulnerable populations.
As the Biden administration responds to the COVID-19 emergency, it should invest in interventions that will make the biggest difference for health at home and abroad. This means bringing US money and know-how back to the international effort to deliver a COVID-19 vaccine worldwide while building back childhood vaccination levels and reestablishing essential services such as antiretroviral therapies and maternal and child health care.
Global health has been relegated to an aid or humanitarian function of US foreign policy
Previous administrations endorsed the importance of global health security in rhetoric and adopted some measures to bolster multilateral health cooperation—most notably the Bush administration’s 2005 International Health Regulations[16] and the Obama administration’s efforts to launch the Global Health Security Agenda[17] and draft a pandemic playbook.[18] Nevertheless, global health security cooperation has largely remained an afterthought in US foreign policy and in those countries most dependent on US development assistance for health. More recently, the Trump administration’s abrupt decision to withdraw from the WHO has led the US to cede a key lever of international influence over global health security at a time when it is most crucial.
The origin and initial spread of COVID-19 within mainland China, an upper-middle-income country receiving no development assistance for health from the United States, was a reminder that global health cooperation cannot be relegated to an “aid” or “humanitarian” issue. To the contrary, global health cooperation and security must be elevated as a key foreign policy priority, fully integrated into US bilateral and multilateral diplomacy and development policy. This will be particularly important over the next two to three years as the US must navigate the high politics of vaccine approval and distribution; gradual relaxation of travel restrictions; and reform of the WHO and other institutions to prevent future pandemics.
The United States must be better prepared to face the next global health threat with a full arsenal of foreign policy tools to identify and address sources of pandemic risk abroad, including health system weaknesses;[19] lapses in data transparency and accuracy;[20] and preparedness against other threats such as antimicrobial resistance;[21] among other issues.
Preparedness for and response to health crises has been underfunded and inadequate
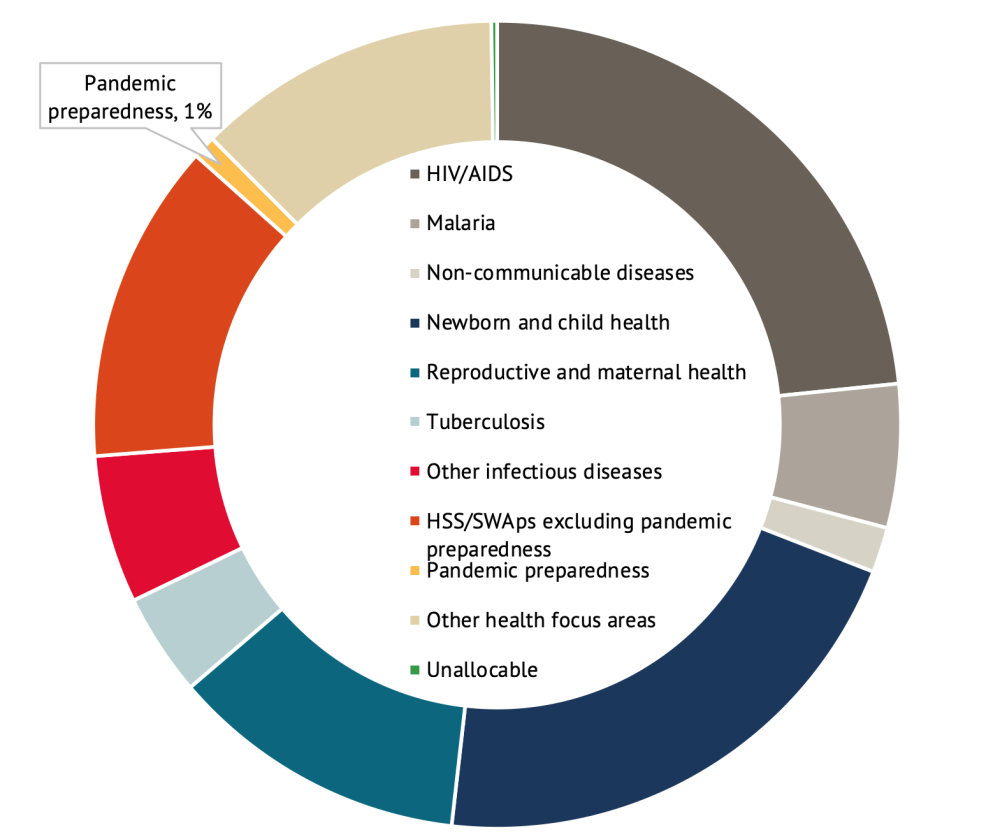
Beyond general US government under-prioritization of global health security, international spending on pandemic preparedness has been routinely inadequate, accounting for less than 1 percent of development assistance for health in 2019 (figure 1).[22] US efforts to support preparedness in low- and middle-income countries have likewise remained small-scale and fragmented across multiple agencies from USAID and CDC to the Departments of State and Defense.[23] Prior to the pandemic, estimates suggested low- and middle-income countries faced a $4.5 billion financing gap for global health preparedness.[24] The COVID-19 pandemic has strained health systems, raising the prospect of even larger gaps in the years ahead.
Figure 1. Development assistance for health by health focus area, 2019
Source: Authors’ calculations using data from the Institute for Health Metrics and Evaluation, Financing Global Health 2019: Tracking Health Spending in a Time of Crisis.
Note: "HSS/SWAps" = Health systems strengthening and sector-wide approaches. "Other health focus areas" = Not identified as allocated to a health focus area listed. "Unallocable" = No information on health focus area. Estimates are preliminary.
Recent crises have revealed fault lines in the US approach to response, recovery, and preparedness for epidemics and pandemics. The 2014-15 West Africa Ebola outbreak illustrated challenges with the US approach to financing and implementing a robust response. While the overall US response was ultimately well-managed, at the outset it was slow to scale, plagued by confusion over roles and responsibilities, and riddled with interagency coordination issues, including between CDC and USAID.[25] The Ebola crisis also underscored the need for longer-term investments in outbreak preparedness in low- and middle-income countries, rather than short-sighted response and recovery efforts when crises arise.[26]
The COVID-19 pandemic has exposed a stark reality: the shortcomings in pandemic response observed during the Ebola crisis were not unique to the developing countries afflicted nor in the slow and disjointed response from the international community. Though some countries, particularly those in East Asia and Taiwan, have mounted admirable control strategies to limit fallout from the COVID-19 pandemic, many wealthy countries with “strong” health systems, including the United States, the United Kingdom, and France, have struggled. Middle-income countries have been among the hardest hit by the pandemic, including our Western Hemisphere neighbors such as Peru, Brazil, Mexico, and Ecuador.
“Vertical” global health investments dominate US aid but are not designed to strengthen health system resilience
US global health investments are primarily appropriated and implemented through a series of “vertical” programs—that is, specific investments intended to address specific health concerns in partner countries. These include the President’s Emergency Plan for AIDS Relief (PEPFAR); the President’s Malaria Initiative (PMI); the US contribution to the Global Fund to Fight AIDS, TB and Malaria; vaccination through Gavi, the Vaccine Alliance; and family planning/reproductive health. These vertical initiatives have saved lives and helped control specific infectious diseases.[27] But by their very nature, vertical programs focus on one specific health concern (or a limited set)—not on building robust and resilient health systems that can reliably and simultaneously address the entire range of infectious diseases, non-communicable illnesses, injuries, and emerging health threats like COVID-19, while maintaining essential services like prenatal care and routine vaccination even in moments of crisis or stress.
While large programs like PEPFAR continued their operations with the help of enduring congressional support, they nonetheless experienced operational challenges—supply chain contract issues,[28] managerial excesses,[29] and data integrity problems[30] that have threatened PEPFAR’s ability to achieve epidemic control and protect the human rights of key populations.
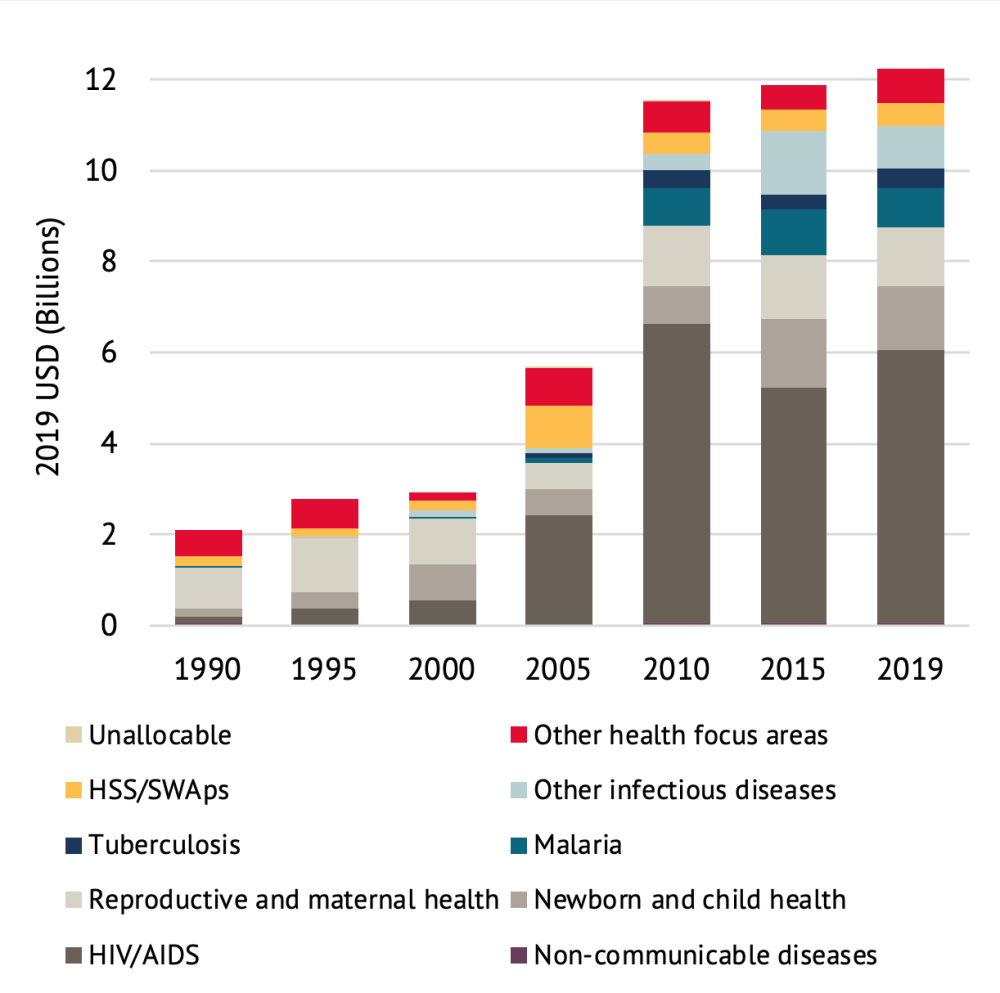
Health systems, in contrast, have seen relative neglect and underinvestment. In 2019, the US provided approximately $500 million for activities intended to strengthen health systems, out of a total of $12 billion in overseas development assistance for health (figure 2).[31] Internationally, the proportion of total development assistance for health used to support health systems has hovered between 15-20 percent since 1990.[32]
Figure 2. Trends in US development assistance for health by focus area, 1990-2019
Source: Authors’ calculations using data from the Institute for Health Metrics and Evaluation, Financing Global Health Viz Hub.
Note: "HSS/SWAps" = Health systems strengthening and sector-wide approaches. "Other health focus areas" = Not identified as allocated to a health focus area listed. "Unallocable" = No information on health focus area.
The vertical organization of most US health assistance also creates siloes, fragmentation, and redundancies, hindering effectiveness. Even where US global health programs support health systems strengthening, most financing is channeled through the vertical funding streams, too often implying a relatively narrow approach designed, first and foremost, to address a single, specific health concern. Yet core health system functions—including data and surveillance systems, the health workforce, laboratory capacity, and supply chains—cut across disease and program areas. The financing and delivery of support to strengthen health systems should reflect this reality.
Further, the goals for and results of health systems strengthening exercises are often weakly defined, creating an accountability vacuum. A 2019 audit from USAID’s Office of the Inspector General found “there is no systematic or reliable way to track what [USAID] missions are obligating and disbursing on [health system strengthening (HSS)] activities” and that “USAID currently has no centralized mechanism for tracking HSS progress at the country level or results of HSS activities across missions.”[33] There have been similar findings for US funding channeled through the multilateral disease-specific agencies such as Gavi,[34] and the Global Fund to Fight AIDS, TB and Malaria. [35]
US-supported programs, as well as those run by national governments, benefit from accurate and timely data and evidence. USAID and CDC have demonstrated leadership in this area through support of the invaluable Demographic and Health Survey (DHS) Program, which generates some of the most reliable data on health statistics in low- and middle-income countries, including infant and maternal mortality. Yet the US and international approach to data and evidence generation have grown increasingly siloed and ad hoc. At times, this renders US agencies unable to clearly demonstrate the results of global health investments (e.g., training activities) and can undermine the cultivation of feedback loops with stakeholders that inform better policy and practice.[36] Many global health funders—the US included—have opted to build and maintain parallel data collection and reporting systems in lieu of the long-term investments in civil registration and vital statistics (CRVS) systems needed to produce reliable, real-time data on births and mortality.[37] Without up-to-date data on basic health statistics, global health programs will struggle to identify and implement the most effective approaches.
The US must shift from a siloed approach to one that preserves results and impact in US trademark global health programs, while also contributing to overall health system performance—health impact, pandemic preparedness, financial protection, responsiveness—for the long-term. All this can be achieved without a complete overhaul—conserving what works and leaning into fill gaps in preparedness and effectiveness.
US multilateral engagement is fractured, limiting policy coherence for global health goals
Global health engagement through multilateral mechanisms offers an opportunity to leverage US funding for broader impact and advance an international agenda towards cross-cutting global health goals. In FY 2019, 19 percent of total US global health investments were allocated through multilateral channels,[38] entitling the US to representation on the respective governing boards. However—and symptomatic of the lack of high-level global health policy coherence and prioritization across the US government—engagement with multilateral health organizations is fragmented with only limited coordination.
A scaled-up and coherent approach to US multilateral engagement will be critical for supporting low- and middle-income countries as they face extraordinary fiscal stress from COVID-19. In the immediate term, governments are experiencing significant economic losses from revenue declines, increasing the pressure on under-resourced health systems.[39]
With some time until an effective vaccine is widely available,[40] the global health community must adjust to the “new normal,” finding ways to deliver effective health programs with a much-reduced footprint abroad. US engagement through multilateral channels will be essential to support allies facing the economic fallout and broader health impacts of the pandemic—even as the US itself is on the road to recovery. In the long term, multilateral engagement should be used to support the broader US strategy for global health engagement and security, formulated and coordinated at the highest levels within the US government.
Policy recommendations
-
Implement the quick wins (see box) to reestablish US credibility, reengage with multilateral global health efforts, and reset partnerships with low- and middle-income countries and the broader global health community.
Quick wins to reestablish US credibility and engagement
- Rejoin the World Health Organization; pay assessed dues; and plan to increase assessed contributions against progress on agreed reforms with emphasis on the organization’s governance and mandate, process and authority to set (and enforce) international health regulations.
- Join COVAX, the effort to finance and commit to providing one or more eventual COVID-19 vaccine(s) to affected lower-income countries and vulnerable populations.
- Prioritize key domestic and global health positions within first round of presidential appointments to restore credibility, including roles at the NSC, HHS, CDC, FDA, USAID, and the Office of the Global AIDS Coordinator. Appointees should have impeccable public health and policy credentials alongside a commitment to evidence-based policies and rigorously measured impact.
- Revoke the “Protecting Life in Global Health Assistance” presidential memorandum that has limited women’s access to safe reproductive health care and contributed to increased induced abortion;[41] and recommit to supporting sexual and reproductive health and rights through both bilateral and multilateral channels.
- Deploy COVID-19 vaccines to all and regain lost ground in childhood vaccination and other essential services to Protect Our World. The exit strategy for the COVID-19 crisis and the opportunity to make large, low-cost, and measurable health gains in the next four years run through scaled-up vaccination. No one is safe until everyone is safe, and the incoming administration should seize the opportunity to join with world leaders in cooperative efforts to ensure widespread distribution of an eventual COVID-19 vaccine. But US leadership will also be vital to reverse troubling health trends and guard against the next global health threat. A top priority should be to work with allies to restore routine childhood immunization, particularly measles which has rebounded to the highest levels seen since 1996, and polio, where eradication efforts have slowed due to under immunization. The COVID-19 vaccination—once available—also provides a unique opening to administer underutilized adult vaccines that protect against cervical cancer and Hepatitis B, helping to reduce heavy and growing disease burdens. In doing so, the US could prevent millions of deaths while restarting economies and laying the groundwork for pandemic preparedness ahead of future threats.
The Biden administration should propose a G7 or G20 deliverable to launch a new effort to Protect Our World via vaccination as the first step of a renewed agenda for global health preparedness.[42] The US already has the necessary partnerships to make this happen with its G7 bilateral partners as well as Gavi, UNICEF, WHO, GPEI, CEPI, Rotary International, the World Bank and multilateral development banks, and other agencies. The challenge is to increase the funding available and make this set of partners work as one in the service of scaled-up and more equitable vaccination with the aim of reaching herd immunity thresholds for childhood vaccination, maximally distributing a low-income country cost-effective COVID-19 vaccine and other adult vaccines, and eradicating polio. Relative roles should be articulated, and the efforts should focus on financing both supply of vaccine as well as addressing delivery and constraints to uptake on both supply and demand sides.
For the COVID-19 vaccine in particular, the US should use multiple strategies: (i) contributing to COVAX and Gavi to pool purchasing for low-income countries; (ii) sharing excess supply from Operation Warp Speed pre-purchases with the rest of the world; (iii) working with the World Bank to enable a contribution to COVAX on behalf of middle-income countries and to support vaccine delivery via World Bank operations;[43] (iv) working with the Pan American Health Organization to assure that Latin American countries, hardest hit to date by COVID-19, have access; (v) encouraging voluntary licensing and tiered pricing arrangements to enable greater manufacture of COVID-19 vaccines and treatments in low- and middle-income countries; and (v) working with COVAX, CEPI and others to pull the development and manufacturing of second- and third-generation vaccines that might be more cost-effective and/or more easily distributed in low- and middle-income countries. - Build an adequately funded global health security architecture that mitigates the impact of future disease and biosecurity threats on human well-being. President-Elect Biden has pledged to take COVID-19 seriously—establishing a task force and developing detailed domestic plans to speed testing and enable rapid deployment of treatments and eventual vaccines. But to prevent a similar pandemic or biosecurity catastrophe from reoccurring, the US must increase strategic investments in outbreak and biosecurity preparedness at home and abroad.
Building off the Global Health Security Agenda and in collaboration with the WHO, a new US initiative is needed to supersize the CDC’s work in disease detection, novel pathogen research, and epidemiological training, and to track outbreaks and drug resistance in humans and animals, around the world, in the public domain, and closer to real-time. Many panels and commissions have proposed different organizational approaches—most have merit, but the key here is to deliver a structure that assures that the US and the world can effectively reduce the probabilities of global spread of a dangerous pathogen as well as prevent new threats like antimicrobial resistance from spiraling out of control.
A key element of this architecture must be dedicated funding for preparedness in low- and middle-income countries.[44] The Biden administration should propose a dedicated global health security initiative that incorporates a multilateral Global Health Security Challenge Fund that creates incentives for countries to collect and share surveillance data as well as dedicate their own resources to preparedness.[45] In the immediate-term, and while an initiative with broader ambitions is set up and established, the Biden administration should work with Congress to secure resources to support the World Bank’s newly established multi-donor Health Emergencies Preparedness and Response Fund,[46] which provides financing to the lowest-income countries to bolster response capacities for COVID-19. US support could help the Fund meet its initial funding target of $500 million (of which it has only raised $130 million to date). - Move towards a health systems approach to funding and cooperation of the trademark US global health programs in HIV/AIDS, malaria, maternal and child health, and family planning. US global health assistance must do a better job of supporting cross-cutting health systems functions while still demonstrating results and impact for trademark US priorities like HIV/AIDS, malaria, TB, and family planning. This is a broad agenda that could include new investments, but there are two near-term actions to take:
First, the Office of the US Global AIDS Coordinator (OGAC) via USAID and CDC should designate at least 20 percent of PEPFAR monies to address identified health system weaknesses and bottlenecks, while retaining incentives for progress on HIV/AIDS results, prioritizing government-to-government assistance and aid modalities that enable more flexible use of funds. Much of US assistance is pre-obligated in existing contracts and cooperative agreements that fund US-based organizations to provide technical assistance and sometimes to deliver services like ARV treatment or bed nets to protect against malaria. This approach is appropriate when partner country governments lack capabilities to safely manage funds or to execute activities; however, in many countries where performance has been good and where the epidemic is waning and US assistance should eventually wind down, it is time to transition to new ways of providing US assistance using government payers, ideally while conserving the high-quality not-for-profit and private providers that PEPFAR has funded for decades. For example, in Kenya, where the US funds upwards of 80 percent of the HIV response, it is time to work more directly with government to share financing burdens and build the capacity to contract or finance existing and new providers directly and to hold them accountable. This approach should be tested but holds promise as a better way to both achieve disease-specific results while providing funding in ways that can strengthen cross-cutting health system functions. There are also opportunities to explore more results-based funding in this space, and CGD has identified detailed strategies to test.[47]
US government support for data collection and reporting should also reinforce a systems orientation. US programs should work to consolidate disease-specific data, surveillance, and analytics into a single, modernized platform—one that can support partner countries to produce general and cause-specific mortality data, strengthen the accuracy of routinely reported administrative data, build on the solid foundations of the Demographic and Health Surveys, and move closer to real-time analytics to inform health policy and program implementation. Better data will also help the US to monitor and evaluate the programs that it supports, including those that are financed through multilateral bodies. All data and evaluations funded directly or indirectly by the US government should be in the public domain by default, with appropriate privacy protections as needed. - Support countries to mitigate the fiscal and economic fallout from the COVID-19 pandemic. Many low- and middle-income countries are experiencing devastating health and economic disruptions from the pandemic; strategic US and multilateral support will be critical to stem losses and restore health, fiscal, and economic stability. In the short term, and in recognition of the extremely constrained fiscal space in many low- and middle-income countries, the US should reassess its posture toward co-financing and transition policies, potentially deferring planned aid transitions in global health to a later date. The US will need to broadly reexamine transition policies and anticipated aid transitions from bilateral programs (e.g., PEPFAR) and multilateral partnerships (e.g., Gavi and the Global Fund). Adjustments should be designed to mitigate declines in available resources and protect hard-won gains in HIV/AIDS, TB, malaria, immunization, and reproductive health.
In the medium-term, the US must view support to economic recovery in low-income countries as a key element of a global health strategy; we know the collateral health effects associated with COVID-19 are as or more important than COVID-19 itself. As such, the multilateral development banks should double their new commitments to enable countries to cope with the acute fiscal crisis ahead.[48] As part of a broader agenda to help countries navigate the fiscal implications of COVID-19, the US should throw its enthusiastic support behind taxes on tobacco, alcohol, and sugar-sweetened beverages. These strategic measures bolster domestic revenue and can help smooth fiscal contraction while simultaneously reducing the health risks associated with cancer, heart disease, and diabetes.[49] Support for health taxes as part of a broader COVID-19 relief package should be extended as a high priority across US diplomatic outreach and multilateral engagement, including via US participation on the governing boards of international financial institutions such as the World Bank and IMF.
Additional reading
Amanda Glassman and Rachel Silverman, 2015. Restructuring US Global Health Programs to Respond to New Challenges and Missed Opportunities. Center for Global Development.
Amanda Glassman and Lauren Post, 2016. Evolving the US Model of Global Health Engagement. Center for Global Development.
Jeremy Konyndyk, 2020. Testimony on COVID-19 and US International Pandemic Preparedness. Testimony before the Senate Foreign Relations Committee, COVID-19 and U.S. International Pandemic Preparedness, Prevention, and Response: Additional Perspectives. June 30, 2020.
Amanda Glassman, 2016. A Progress Report on the West Africa Ebola Epidemic. Testimony before the Senate Foreign Relations Committee Subcommittee on Africa and Global Health Policy. April 7, 2016.
Jeremy Konyndyk, 2019. Struggling with Scale: Ebola’s Lessons for the Next Pandemic. Center for Global Development.
Jeremy Konyndyk, 2019. The Dos and Don’ts of USG Humanitarian Reorganization. CGD Note, Center for Global Development.
Thanks to Brin Datema for graphics and help with references.
[1] Y-Ling Chi, Lydia Regan, Cassandra Nemzoff, Carleigh Krubiner, Yasmine Anwar, and Damian Walker, 2020. Beyond COVID-19: A Whole of Health Look at Impacts During the Pandemic Response. CGD Policy Paper 177. Center for Global Development.
[2] Institute for Health Metrics and Evaluation (IHME), 2020. Financing Global Health 2019: Tracking Health Spending in a Time of Crisis.
[3] Kaiser Family Foundation, 2019. The U.S. Government and Global Health.
[4] Katie Rogers and Apoorva Mandavilli, “Trump Administration Signals Formal Withdrawal From W.H.O.,” The New York Times, July 8, 2020; Amanda Glassman and Brin Datema, 2020. What is the World Health Organization without the United States. CGD Blog. Center for Global Development.
[5] Lena H. Sun, “Top White House official in charge of pandemic response exits abruptly,” The Washington Post, May 10, 2018.
[6] US Government Accountability Office, 2020. Global Health Assistance: Awardees' Declinations of U.S. Planned Funding Due to Abortion-Related Restrictions; US Agency for International Development, 2020. Acting Administrator John Barsa Letter to UN Secretary General Guterres. Press Release, May 18, 2020.
[7] Emily Rauhala and Yasmeen Abutaleb, “U.S. says it won’t join WHO-linked effort to develop, distribute coronavirus vaccine,” The Washington Post, September 1, 2020.
[8] Y-Ling Chi, Lydia Regan, Cassandra Nemzoff, Carleigh Krubiner, Yasmine Anwar, and Damian Walker, 2020. Beyond COVID-19: A Whole of Health Look at Impacts During the Pandemic Response. CGD Policy Paper 177. Center for Global Development.
[9] Global Polio Eradication Initiative (GPEI), 2020. Call to Action for Measles and Polio Outbreak Prevention and Response.
[10] Roxanne Oroxom and Amanda Glassman, 2019. Vaccine Introduction and Coverage in Gavi-Supported Countries 2015-2018: Implications for Gavi 5.0. CGD Note. Center for Global Development.
[11] Amanda Glassman and Liesl Schnabel, 2019. Gavi Going Forward: Immunization for Every Child Everywhere? CGD Blog. Center for Global Development.
[12] Roxanne Oroxom and Amanda Glassman, 2019. Vaccine Introduction and Coverage in Gavi-Supported Countries 2015-2018: Implications for Gavi 5.0. CGD Note. Center for Global Development.
[13] Global Polio Eradication Initiative (GPEI), 2020. Call to Action for Measles and Polio Outbreak Prevention and Response.
[14] Kaiser Family Foundation, 2020. The U.S. Government and Global Polio Efforts.
[15] Amie Batson, Awi Federgruen, Nirmal Ganguly, Amanda Glassman, Simba Makoni, and Stanley Plotkin, forthcoming. “Polio Eradication Vaccine Investment – How do we ensure polio vaccines are available to keep the world polio free after transmission of WPV has been interrupted,” Globalization and Health.
[16] World Health Organization, n.d. International Health Regulations.
[17] See: Global Health Security Agenda (GHSA) website; US Department of State, 2020. Strengthening Health Security Across the Globe: Progress and Impact of U.S. Government Investments in the Global Health Security Agenda. 2019 Annual Report.
[18] Dan Diamond and Nahal Toosi, “Trump team failed to follow NSC’s pandemic playbook,” Politico, March 25, 2020.
[19] Angela E. Micah, Katherine Leach-Kemon, and Joseph L Dieleman, 2020. Health-Systems Strengthening in the Age of COVID-19. Think Global Health; Pandemic Action Network, 2020. Break the Cycle of Panic and Neglect: Preventing the Next Pandemic.
[20] Global Health Security Architecture and Governance Working Group, 2020. The Next Pandemic Won’t Wait: An Agenda for Action to Strengthen Global Preparedness. Pandemic Action Network; Global Preparedness Monitoring Board, 2020. A World in Disorder. Global Preparedness Monitoring Board Annual Report 2020. World Health Organization.
[21] Kimberly Ann Elliott, 2015. Antibiotics on the Farm: Agriculture’s Role in Drug Resistance. CGD Policy Paper 059. Center for Global Development; Janeen Madan Keller, Kimberly Ann Elliott, and Charles Kenny, 2017. Onwards and Upwards: Strengthening Global Cooperation to Address Antimicrobial Resistance. CGD Blog. Center for Global Development.
[22] Institute for Health Metrics and Evaluation (IHME), 2020. Financing Global Health 2019: Tracking Health Spending in a Time of Crisis.
[23] Kaiser Family Foundation, 2019. The U.S. Government and Global Health.
[24] CSIS Commission on Strengthening America’s Health Security, 2019. Ending the Cycle of Crisis and Complacency in U.S. Global Health Security. Center for Strategic and International Studies.
[25] Jeremy Konyndyk, 2019. Struggling with Scale: Ebola’s Lessons for the Next Pandemic. CGD Report. Center for Global Development.
[26] Amanda Glassman, 2016. A Progress Report on the West African Ebola Epidemic. Testimony before the Senate Foreign Relations Committee Subcommittee on Africa and Global Health Policy. April 7, 2016.
[27]Institute of Medicine, 2013. Evaluation of PEPFAR. The National Academies Press; President’s Malaria Initiative, 2012. External Evaluation of the President's Malaria Initiative.
[28] Michael Igoe, “Exclusive: Documents reveal largest USAID health project in trouble,” Devex, August 25, 2017.
[29] Michael Igoe, “PEPFAR teams complain of 'dictatorial,' 'directive,' and 'autocratic' leadership,” Devex, February 14, 2020.
[30] Charles Piller, “The inside story of how Trump’s COVID-19 coordinator undermined the world’s top health agency,” Science Magazine, October 14, 2020.
[31] Data from Institute for Health Metrics and Evaluation (IHME) Financing Global Health Viz Hub.
[32] Angela E. Micah, Katherine Leach-Kemon, and Joseph L. Dieleman, 2020. Health-Systems Strengthening in the Age of COVID-19. Think Global Health.
[33] Office of the Inspector General for the US Agency for International Development, 2019. More Guidance and Tracking Would Bolster USAID's Health Systems Strengthening Efforts.
[34] Cordelia Kenney and Amanda Glassman, 2019. Gavi’s Approach to Health Systems Strengthening: Reforms for Enhanced Effectiveness and Relevance in the 2021–2025 Strategy. CGD Note. Center for Global Development.
[35] Technical Evaluation Reference Group, 2019. Technical Evaluation Reference Group (TERG) Thematic Review to Assess the Current Approach to Investments in Resilient and Sustainable Systems for Health (RSSH). Final Report. The Global Fund to Fight AIDS, Tuberculosis and Malaria; Technical Evaluation Reference Group, 2017. Final Report The Global Fund to Fight AIDS, Tuberculosis and Malaria Strategic Review 2017. The Global Fund to Fight AIDS, Tuberculosis and Malaria.
[36] Office of the Inspector General for the US Department of State, 2019. Audit of Cooperative Agreement Sub-Award Recipients Supporting the U.S. President’s Emergency Plan for AIDS Relief.
[37] Amanda Glassman, 2020. What Matters Most for COVID-19 Policy Now: Better Mortality Data. CGD Blog. Center for Global Development.
[38] Kellie Moss, Josh Michaud, and Jennifer Kates, 2019. The U.S. Government and Multilateral Global Health Engagement: 5 Key Facts. Kaiser Family Foundation.
[39] Adrian Gheorghe, Kalipso Chalkidou, Amanda Glassman, Tomas Lievens, and Anthony McDonnell, 2019. COVID-19 and Budgetary Space for Health in Developing Economies. CGD Note. Center for Global Development.
[40] Anthony McDonnell, Robert Van Exan, Steve Lloyd, Laura Subramanian, Kalipso Chalkidou, Adrian La Porta, Jiabin Li, Eddine Maiza, David Reader, Julie Rosenberg, Jack Scannell, Vaughan Thomas, Rebecca Weintraub, and Prashant Yadav, 2020. COVID-19 Vaccine Predictions: Using Mathematical Modelling and Expert Opinions to Estimate Timelines and Probabilities of Success of COVID-19 Vaccines. CGD Policy Paper 183. Center for Global Development.
[41] Amanda Glassman, 2017. Zombie Policy on International Family Planning Rises Again. CGD Blog. Center for Global Development; Boniface Ayanbekongshie Ushie, Kenneth Juma, Grace Kimemia, Maggie Magee, Emily Maistrellis, Terry McGovern, and Sara E. Casey, 2020. “Foreign assistance or attack? Impact of the expanded Global Gag Rule on sexual and reproductive health and rights in Kenya,” Sexual and Reproductive Health Matters 28(3): 1-16; Nina Brooks, Eran Bendavid, and Grant Miller, 2019. “USA aid policy and induced abortion in sub-Saharan Africa: an analysis of the Mexico City Policy,” The Lancet Global Health 7(8): e1046–53.
[42] Amanda Glassman, “Protect our world: How the Biden administration can save lives and economies worldwide,” The Hill, November 23, 2020.
[43] Kalipso Chalkidou, Prashant Yadav, and Amanda Glassman, 2020. Making the $12 Billion Go Further: Four Things the World Bank Can Do in Support of COVID-19 Vaccination Efforts. CGD Blog. Center for Global Development.
[44] Global Health Security Architecture and Governance Working Group, 2020. The Next Pandemic Won’t Wait: An Agenda for Action to Strengthen Global Preparedness. Pandemic Action Network.
[45] Center for Global Development, Center for Strategic and International Studies, Georgetown University, and Nuclear Threat Initiative, 2020. Concept Note: Global Health Security Challenge Fund.
[46] World Bank Group, 2020. World Bank Group to Launch New Multi-donor Trust Fund to Help Countries Prepare for Disease Outbreaks. Press release, April 17, 2020.
[47] Amanda Glassman and Rachel Silverman, 2016. Next Generation Financing for Global Health: What, Why, When, How?. CGD Brief. Center for Global Development; Mead Over and Amanda Glassman, 2015. Strengthening Incentives for a Sustainable Response to AIDS: A PEPFAR for the AIDS Transition. CGD Brief. Center for Global Development.
[48] Masood Ahmed, 2020. Beyond the Numbers: Why the World Needs a More Ambitious MDB Response to COVID-19. CGD Blog. Center for Global Development.
[49] Task Force on Fiscal Policy for Health, 2019. Health Taxes to Save Lives: Employing Effective Excise Taxes on Tobacco, Alcohol, and Sugary Beverages. Bloomberg Philanthropies.
Rights & Permissions
You may use and disseminate CGD’s publications under these conditions.