Recommended
CGD’s COVID-19 Gender and Development Initiative
As donor institutions and governments seek to provide relief and support recovery from the COVID-19 pandemic and global recession, CGD’s COVID-19 Gender and Development Initiative aims to ensure that their policy and investment decisions equitably benefit women and girls. We seek to support decision-makers in understanding the gendered impacts of the COVID-19 pandemic; assess health, economic, and social policy response measures with a gender lens; and propose evidence-based solutions for an inclusive recovery. Recognizing that the dialogue to date has largely emphasized challenges facing women and girls in high-income settings, our analysis centers on women and girls in low- and middle-income countries.
In this policy brief, we summarize the findings of a CGD working paper, Addressing the COVID-19 Crisis’s Indirect Health Impacts for Women and Girls. We examine how the pandemic is affecting women’s and girl’s health, including their sexual and reproductive health; some of the ways national governments and donor institutions have sought to maintain the provision of essential health services; and existing gaps, opportunities, and promising strategies donors and governments should pursue to address indirect harms to women’s and girl’s health during and beyond the COVID-19 crisis.
What is the problem?
When health crises like COVID-19 emerge, the simultaneous shocks to economic, social, and health systems can have different implications for women and girls, with gendered impacts across various dimensions of wellbeing—including indirect impacts on health. Looking across a few key health services, with a special focus on sexual and reproductive health services, the limited data available showed that the magnitude and duration of disruptions to essential services vary widely across different countries, as did initial impacts on health outcomes.
Contraception and abortion services. Whereas Kenya had only minimal disruption of services, India appeared to have much larger disruption to contraceptive services across all methods, with the largest reductions in IUDs and injectables. Nigeria had more moderate documentation of disruption (10-15 percent in April and May), but this might be more indicative of the low coverage of modern contraceptives prior to the pandemic and the possibility that the pandemic stalled important progress that was being made in early 2020 to expand family planning services.
Maternal health care. Across countries, there was variable disruption in utilization and access to facility-based deliveries. Countries like India and Nepal documented much larger reductions in attended births, as well as increases in adverse maternal and neonatal outcomes, as compared to the minimal disruptions reported in Kenya. Evidence indicates greater and more prolonged impacts on antenatal care (ANC) visits across several countries. Disruptions to ANC can be especially problematic given missed opportunities to address iron deficiency and undernutrition, as well as implications for HIV diagnosis and prevention of mother-to-child transmission.
HIV. UNAIDS data on HIV testing of pregnant women across 17 countries show decreases in nearly all countries during the early months of the pandemic, with most rebounding to pre-pandemic levels by June or July (except Indonesia, Botswana, and Sierra Leone). Among the 15 countries reporting on treatment among pregnant women living with HIV, all but five have recovered to the February numbers of women receiving treatment (except Botswana, South Africa, Sierra Leone, Togo, and Guatemala).
Violence against women and girls. In a review of 74 studies documenting the impact of the pandemic on violence against women and children, nearly half found an increase in violence against women during COVID-19, and another 25 percent reported mixed results with an increase in at least one measure of violence. Service providers report facing additional constraints to supporting survivors. Where studies observe mixed findings or decreases, there are concerns that much of this is due to underreporting, as victims are less able to report violence and seek help under lockdown conditions.
Impacts on mental health. In a review of 98 studies across diverse geographic settings that compared mental health status and outcomes between men and women during the COVID-19 pandemic, over 80 percent indicated that women were experiencing greater adverse mental health effects—including higher levels of stress, anxiety, depression, and fear of COVID-19 than men. Several studies have also indicated disproportionate mental health impacts among female health workers compared to their male counterparts, as well as exacerbated mental health issues for pregnant women during the pandemic.
The emerging evidence on the gendered effects of the COVID-19 pandemic has a number of limitations, with challenges in data access, quality, and interpretation. The studies use different data sources, ranging from routine health information systems and administrative data from facilities to rapid phone surveys, and analyses employ different methodological approaches and comparators to assess changes in utilization or specific outcome measures. Cross-country comparisons are also challenging given the different starting points of health systems before the pandemic, as well as the epidemiological variation with regard to COVID-19 burden of disease and the corresponding response strategies used in different settings.
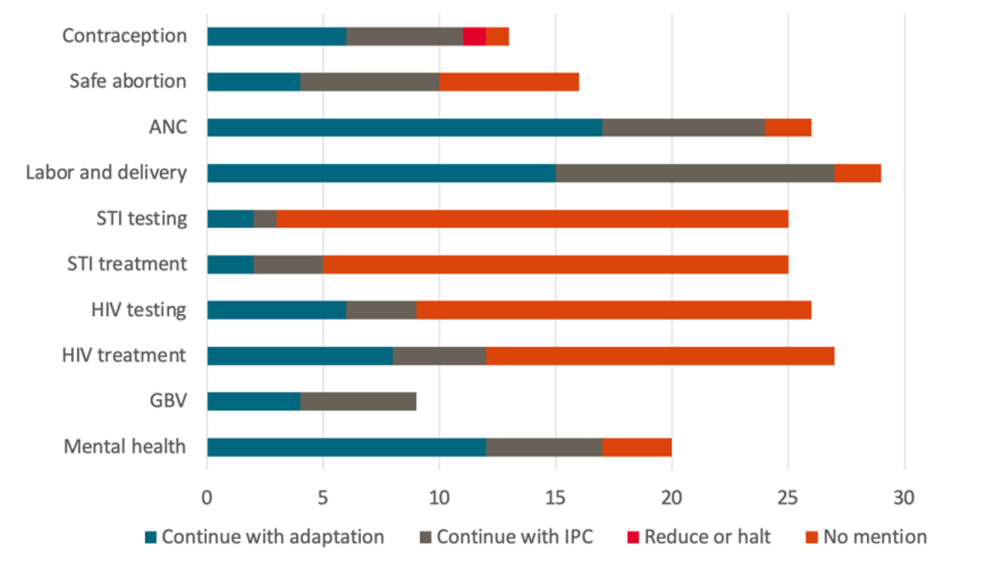
Figure 1. Adaptations to essential health services
What are policymakers and donors doing in response?
Some national governments have sought to maintain the provision of essential health services through modifications. Using the PATH/WHO COVID-19 Essential Health Services Policy Tracker—which contains information on over 200 policy documents spanning 119 countries—we examined the extent to which policy documents advised continuation of service with additional adaptation (e.g., telehealth), continuing services with Infection Prevention and Control (IPC), reducing or halting health services, or did not mention the health service, specifically looking across the health service areas outlined above.
Many countries are continuing to offer essential services, relying on adaptations such as telehealth, reduced facility-based care, or shorter hospital stays in favor of community or home-based care, use of scheduling systems to space out appointments, and multi-month dispensing of medications—with many more relying solely on IPC to reduce the COVID-19 risk. However, there is variability across health areas, with greater documented approaches to maintain maternal care and family planning services as compared to testing and treatment of HIV and other STIs. Additionally, many countries have internal inconsistencies between different policy documents and guidelines, with adaptations either unspecified or overly reliant on telehealth measures that may not reach populations without adequate mobile phone or internet access. More is needed to understand the implementation and impact of adaptations.
Additionally, the United Nations Development Programme and UN Women are tracking the gender-sensitivity of COVID-19 policy responses from national governments and territories. The most systematically documented measures relevant to indirect health effects focus on violence against women and girls, constituting 71 percent of all gender-sensitive policy measures the tracker documents across 135 countries.
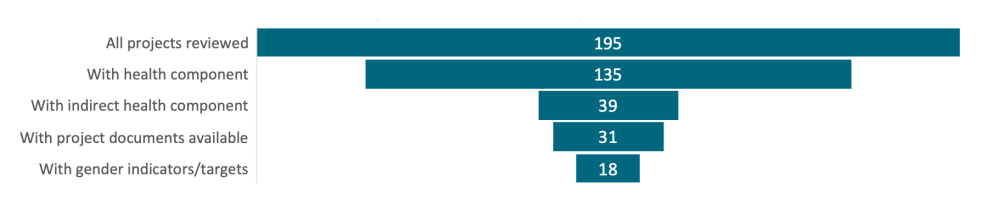
Donor institutions are working to protect and promote essential health services during COVID-19 through knowledge generation and sharing, modifying existing programs to adapt to the COVID-19 context, and launching new investments to address COVID-specific challenges. Various donor organizations have leveraged their data systems and platforms to shed light on disruptions to service delivery, including the Global Financing Facility and Global Fund—but beyond blog posts and press releases, full details and data are often not published in the public domain. With regard to new investments, in reviewing project documents from the World Bank, the African Development Bank, and the Asian Development Bank, the vast majority of new health projects launched in response to COVID-19 focus exclusively on the direct health impacts of COVID-19 disease. Only 39 out of 135 total health projects contain a component that addresses the indirect health impacts of the COVID-19 crisis, and just over half of these included gender-specific indicators. The few with a gender dimensions largely focused on addressing gender-based violence, maternal health, and broader gender-sensitive health support. Deeper analysis is needed to understand the impact of specific targets, including those incentivized through results-based approaches, in driving coverage and equity outcomes.
Figure 2. MDB project documents’ attention to indirect health impacts & gender
What else is needed?
Our review of the indirect health impacts of COVID-19, and the efforts governments and donor institutions have made to date to address these impacts, suggest six areas of opportunity for future action:
- Improve data collection and sharing, with explicit attention to gender and intersectional disadvantage. Donor and policymakers should ensure standard collection of sex- and age-disaggregated data, but also other factors such as location, socioeconomic status, and ethnicity that can compound disadvantage in both COVID-19 efforts and in broader initiatives to strengthen health information infrastructures for timely, local health data. Data collection approaches cannot rely solely on methods likely to disproportionately exclude women, especially the most marginalized women, such as mobile phone surveys.
- Evaluate what works to mitigate gendered indirect effects, especially integrated approaches—and hold governments and organizations accountable to data use and transparency to inform and adapt their efforts. More work is needed to assess the implementation of various strategies and policies to mitigate indirect health impacts of the crisis, including effectiveness, feasibility, acceptability, and sustainability of programs and adaptations. There are also important opportunities to evaluate integration of health programs and other social support programs within a “one-stop-shop” model, to understand how complementary offerings may address the multiple needs of women and girls during a crisis while alleviating the burden on them to seek out support from multiple sites. Decisions to reallocate resources should be critically evaluated, particularly when the indirect harms caused may exceed the benefits related to pandemic response.
- Build on the momentum of health innovations that COVID-19 has generated. The COVID-19 pandemic is giving rise to a surge of new locally adapted innovations and momentum for scale-up of existing innovations, such as self-care SRH products, telehealth platforms, and new product delivery systems—all of which have the potential to enable women and girls to more readily access healthcare conveniently and safely. However, new digital models and tools need to be integrated into the larger health system to harness their full potential and avoid exacerbating existing inequities. Blended funding flows from governments, development partners, and private sector can better connect digital tools with national health systems, potentially channeled through demand-side financing mechanisms to build healthcare around the choices, preferences, and agency of women and girls as users.
- Leverage health reforms to enhance women’s and girls’ agency, choice and equitable access. Wherever feasible, support for women’s and girls’ health initiatives should go towards national health systems as opposed to creating parallel systems at the expense of coherent, sustainable financing structures. Overly fragmented operations and funding flows, even when targeted towards specific groups of women and girls, risk undermining cost, access, and equity goals. Development partners should support and incentivize governments to protect public spending for—and equitable coverage of—the most cost-effective services, including sexual and reproductive healthcare, and promote family planning as part of the universal health coverage agenda.
- Prioritize support for women as leaders and providers in the global health workforce. Although women constitute over 70 percent of the global health workforce, they hold only 25 percent of leadership roles. COVID-19 decision-making bodies and expert task forces have not performed well on basic measures of gender parity, let alone inclusion of women of color and representation from the Global South. Women need greater representation in leadership and decision-making roles across the health sector. Furthermore, women health workers on the front line need greater safety, support, and appropriate compensation. This is particularly true for community health workers who are often underpaid or unpaid, and sent into communities without adequate personal protective equipment.
- Elevate women and girls as members of civil society. Governments and donors should create space for civil society input, working toward a positive legacy of the COVID-19 crisis with regard to open and accountable global health governance that includes the needs and perspectives of women and girls. The 2021 Generation Equality Forum offers an opportunity to engage with civil society and formulate concrete commitments collaboratively.
This brief is based on the CGD working paper Addressing the COVID-19 Crisis’s Indirect Health Impacts for Women and Girls. To read the full paper, including citations, please visit cgdev.org/covidandgender
Rights & Permissions
You may use and disseminate CGD’s publications under these conditions.